OralScan, invented by Subhash Narayanan, is a non-invasive optical device that detects oral cancer quickly and at a low cost without a biopsy.
Reinventing healthcare
By Raghunath Mashelkar
A major outbreak of dengue fever in India in 2013 resulted in a flood of patients at hospitals and clinics across the country. As their numbers soared, test kits for quickly identifying dengue so as to begin treatment early went out of stock.
The test kits were imported and though an order had been placed with a South Korean firm to replenish them, the consignment was sent to Africa instead by mistake!
Attention then shifted to a test invented by Indian scientists. It had for long been overlooked in favour of the imported tests which were widely used and dominated the market.
The Indian test was called Dengue Day 1 because it could detect dengue within minutes on the first day of the fever. It could also differentiate between primary and secondary dengue virus infections, which is vital for the clinical management of a patient. The test could also detect the presence of the virus in the Aedes mosquito.
Importantly, it was three to four times cheaper than the conventional test and could be used in resource-poor settings. In other words, it could be easily used in villages and small towns where health infrastructure was inadequate.
All in all, Dengue Day 1 was a much better option than the imported tests which had been in use. But it wasn’t a trusted product because it had been invented in India and not abroad. It, therefore, had little or no presence at all in the Indian public healthcare system despite its many advantages.
But during the 2013 outbreak, there was a huge unmet demand for test kits. There was also no other option since the imported tests were out of stock. And Dengue Day 1 finally got the attention it deserved and was widely employed.
From being ignored, Dengue Day 1 went on to capture 75 percent of the Indian market because it was cheaper, superior and better suited to Indian conditions. Since then, it has been used for doing 10 million tests. Other countries have begun importing it.
The Dengue Day 1 test is a great example of ‘inclusive innovation’, a cause I have been passionately championing. Simply put, inclusive innovation makes high technology affordable and leverages it for the poor, especially in rural areas where health facilities are sorely lacking.
Vast numbers of Indians continue to be poor. Around 70 percent of the population lives in rural areas but they don’t have access to even 30 percent of the nation’s health infrastructure. Just three percent of Indian doctors are located in rural areas and the doctor-patient ratio is 1:2,000. There are merely eight hospital beds for a population of 10,000 whereas China, by comparison, has 40 for the same number of people. There should be 44 health workers per 10,000 of population, but India has only 22.
 |
|
Dr Navin Khanna |
These and other similarly depressing figures are well known. They tell a story of extreme neglect of public healthcare systems. The question is how to quickly improve medical facilities and provide easy and equal access to them so as to build a healthy nation even as roads, power lines and the internet reach remote corners of India.
Providing health facilities and putting in place more doctors, nurses and health workers will take time and investments. There is also a complex management problem to contend with. Both the central and state governments have generally sound public healthcare policies. The healthcare system is well structured, from small sub-centres to primary health centres and secondary and tertiary hospitals. But the system lacks sophistication and doesn’t deliver uniform results.
Until the system is made more efficient, can ‘inclusive innovation’ be used to leapfrog to higher standards of healthcare? Can we simultaneously pursue ‘affordable excellence’ through technological innovations which give the poor the highest quality of healthcare?
Can we do it? Generally, what is affordable is not excellent and what is excellent is not affordable. This is where inclusive innovation becomes important — getting more (performance) by using less (resources) for more (people). More from less for more (MLM).
I have for long been a proponent of the concept of ‘Gandhian Engineering’, which to me means getting more from less for more people and not just for more profit.
We have seen that inclusive innovations provide instant benefits to people. They also deliver bigger and long-term healthcare outcomes. Perhaps they could also be triggers for creating demand for better healthcare services in general and jolting the system out of its current inertia.
The ultimate goal should be ‘affordable excellence’ in healthcare so that even as systemic transformations are awaited, the highest quality of medical care is made available to the rich and poor alike.
Taking the highest standards of healthcare to the poor is particularly important because it empowers them to compete and reverse generations of inequality. To move forward, people need to first be healthy.
Innovations, however, don’t come off the shelf. They have as much to do with technological prowess and talent as happenstance and personal experience. For most innovators the innovation is the endpoint of a journey.
Work on Dengue Day 1, for instance, was begun by Dr Navin Khanna at the International Centre for Genetic Engineering and Biotechnology with funding from the Defence Research and Development Organization. But since DRDO’s terms of funding were restrictive, an alternative test was created and patented. Thereafter, the test languished until the big dengue outbreak and the South Korean ship mistakenly taking the consignment of dengue test kits to Africa. What if the ship had come to India?
Inclusive innovation is really entrepreneurship at its best. It needs to be nurtured in a social and economic framework which recognizes its huge potential to deliver better healthcare and simultaneously deepen and broaden existing markets through revolutionary price points and transactions that serve the poor.
Eleven years ago we started the Anjani Mashelkar Inclusive Innovation Award (AMIIA) in memory of my mother. She brought me up, facing all the odds that an extremely poor and uneducated widow moving to Mumbai with her only child — a six-year-old boy — would face. And this she did with courage and dignity.
When she passed away, we found all the money that was given to her for her small personal expenses from time to time over the years tucked away in her cupboard with a note that said: ‘Use this money to do science for the poor.’
Since then, the award in her name is given each year at the inauguration ceremony of the annual National Inclusive Innovation Conference on November 17, the day she left us.
With its decade-long journey now, the award has been recognizing stellar inclusive innovations that have managed to solve the problems that need to be solved as opposed to those that can be solved. These innovations were born of the minds and hearts of compassionate innovators who sometimes left their cushy careers to dedicate their lives to improving quality of life for the disadvantaged. They connected the dots, applied the most advanced technology, reimagined delivery and in the process reinvented healthcare models.
Dengue Day 1 was one of the awardees. But let me introduce you to the others and their amazing journeys:
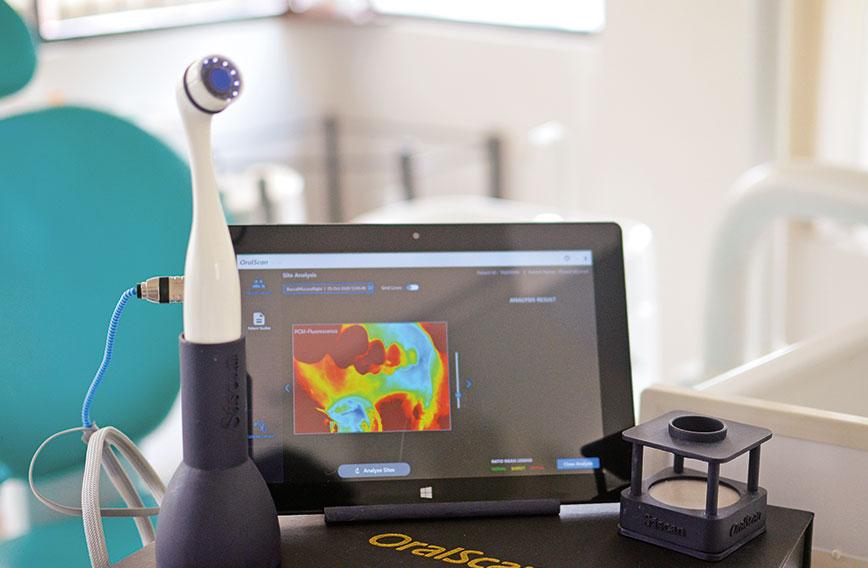
OralScan: Optical device detects oral cancer early at low cost and without a biopsy
As with all cancers, oral cancer has to be detected early for treatment to be successful. But it is not easy to visually detect changes in the tissues in the oral cavity. A doctor using a torch can at best have a subjective assessment and as a result diagnosis can be way off the mark.
 |
|
Subhash Narayanan |
 |
Cancer can be confirmed through a biopsy, but it is expensive and can also be painful for a patient when multiple tissue samples have to be collected. For biopsies to be accurate, tissues have to be collected from the most malignant site in the lesion.
The problem multiplies when you are in a rural area. Lack of proper diagnostic equipment, doctors and technicians means people have to travel to the nearest town.
Dr Subhash Narayanan, founder of Sascan Meditech, has invented OralScan, a breakthrough device that provides early, accurate and cost-effective detection of pre-cancerous lesions.
OralScan uses an optical system with custom-built software and algorithms for tissue analysis. It enables the physician to visualize and discriminate between healthy and potentially malignant sites.
With good accuracy, 97 percent sensitivity and 92 percent specificity, the technician or the doctor can easily detect cancer and eliminate the need for a biopsy. If there is any suspicion of cancer, OralScan pinpoints the site from which the tissue for a biopsy should be taken. This eventually saves the patient the pain of multiple biopsies and the associated costs.
OralScan is currently being used for screening and early detection of oral cancer in seven hospitals and dental colleges. So far, it has been used for screening thousands of patients in remote villages in Karnataka, Kerala, Maharashtra and Arunachal Pradesh.
Dr Narayanan’s mother was wrongly diagnosed with cancer. Driven by his personal experience, he took up the challenge to make diagnosis less subjective and invasive.
He worked as a research scientist at the Centre for Earth Science Studies in Thiruvananthapuram from 1980 to 2013.
During his scientific career, he had gained deep expertise in biophotonics, optical spectroscopy and multispectral imaging. He started working on this innovation in 2005 and prototyped his system.
iBreastExam: Non-invasive and affordable, it makes breast cancer screening easy
In 2007, a young Mihir Shah was about to get married when his soon-to-be mother-in-law was diagnosed with breast cancer. She underwent chemotherapy and survived, wearing a wig to the wedding. This experience led to Shah setting up UE LifeSciences along with co-founders Matthew Campisi and Bhaumik Sanghvi.
 |
|
Mihir Shah |
 |
When they started to dig deeper, they learnt that over 90 percent of women in the developing world did not have access to any mechanism for early detection of breast cancer. In India a woman is detected with breast cancer every four minutes.
The incidence of the disease in India is on the rise in both rural and urban areas and there is a huge unmet need for quick and early detection, which is the best way improve outcomes from treatment. To meet this need they came up with iBreastExam, an early screening device for breast cancer. Early detection is the best way to improve outcomes from the treatment of breast cancer.
iBreastExam uses innovative sensor and material technology combined with software computing to accurately identify cancerous lesions and tumours. This breakthrough technology has the potential to dramatically improve the accessibility and affordability of breast cancer screening. It is portable, radiation-free and non-invasive. It has been approved by the FDA in the US, ensuring that the screenings are safe, pain-free and private.
They have also proposed an innovative pay-per-use model — instead of targeting direct sales — which allows doctors in every corner of the country to start screening women for breast cancer at the earliest.
iBreastExam has reached over 350,000 women in 12 countries. With devices currently on the market, over one million women will soon receive a safe, affordable and radiation-free breast exam in the convenience of a community health centre or their homes.
The second-generation iBreastExam sensor technology has improvements (spatial resolution, data frequency, power consumption, ease of use, clinical efficacy) by orders of magnitude over the first-generation technology, helping expand access to many more women globally.
In 2017, GE Healthcare announced a distribution partnership with UE LifeSciences to take iBreastExam to women in 25 countries. UE LifeSciences has also forged strategic partnerships with big pharma and leading medical device distribution channels. Recently, it entered into a distribution agreement with Siemens Healthineers for the US market. The World Bank and IMF have rightly recognized their innovation with the prestigious 2022 Global Women’s HealthTech Award.
Sanket: ECG device, size of a credit card, records readings on a smartphone
 |
 |
|
Rahul Rastogi |
Neha Rastogi |
When Rahul Rastogi’s father was admitted to hospital after complaining of a heavy feeling in his chest, tests showed he had been on the brink of a massive heart attack. That near-crisis and the stress of regular follow-up tests after the angioplasty made Rahul and his wife, Neha, ponder if heart monitoring could be done differently.
 The Rastogis developed Sanket, an ECG recorder, which makes monitoring the heart as simple as taking body temperature. It is low-cost and extremely portable, being the size of a credit card. It has 12 leads and connects to a smartphone wirelessly, displaying and recording ECG graphs, also on a smartphone. The ECG report can be shared instantly with a doctor via email, Bluetooth — and even WhatsApp!Both were electronics engineers by education and working as engineers at well-known multinational corporations, CSC and Samsung. They decided to quit their jobs to create a gadget to help people monitor their heart function on their own at home, hence providing early warning of a crisis. With nearly 30 million people suffering from heart ailments, India is unfortunately known as the heart disease capital of the world. Heart attacks are also notoriously difficult to detect.
The Rastogis developed Sanket, an ECG recorder, which makes monitoring the heart as simple as taking body temperature. It is low-cost and extremely portable, being the size of a credit card. It has 12 leads and connects to a smartphone wirelessly, displaying and recording ECG graphs, also on a smartphone. The ECG report can be shared instantly with a doctor via email, Bluetooth — and even WhatsApp!Both were electronics engineers by education and working as engineers at well-known multinational corporations, CSC and Samsung. They decided to quit their jobs to create a gadget to help people monitor their heart function on their own at home, hence providing early warning of a crisis. With nearly 30 million people suffering from heart ailments, India is unfortunately known as the heart disease capital of the world. Heart attacks are also notoriously difficult to detect.
Sanket does away with expensive ECG machines, distant hospitals or laboratories and skilled technicians. It has over 200,000 users.
Their organization, Agatsa, has evolved to serve not only India, but Turkey, Germany, the US, Brazil, Australia, Malaysia, Bangladesh and the UAE.
ToucHb: Non-invasive anaemia check gives on-the-spot readings from anywhere
 |
 |
|
Myshkin Ingawale |
Abhishek Sen |
Iron-deficiency anaemia is a significant health crisis among women in India. It is recommended that pregnant women get a haemoglobin (Hb) check done every three months during pregnancy.
Unfortunately, some patients may live at a distance of up to 15 miles from a primary health centre. Travelling this distance is not only uncomfortable for them, it also leads to the loss of a day’s wages. The invasive method of pricking the finger to draw blood is an unpleasant experience as well.
Myshkin Ingawale, an IIM Calcutta alumnus, has invented a handheld, non-invasive device called TouchHb to measure haemoglobin.
His invention went through as many as 32 iterations before Ingawale was satisfied with its performance. He and Abhishek Sen are now co-founders of Biosense Technologies.
 TouchHb is a portable, battery-operated device which can produce an on-the-spot reading without a prick. The patient simply has to place a finger in the clip or probe. The readings are available within 60 seconds!
TouchHb is a portable, battery-operated device which can produce an on-the-spot reading without a prick. The patient simply has to place a finger in the clip or probe. The readings are available within 60 seconds!
It works using optical technique photoplethysmography (PPG) where light of different wavelengths is shone through skin tissue. This helps in understanding the concentration of haemoglobin in the tissue. No special skills are needed to use this device.
Since there is no need for needles, lancets, micro-cuvettes, blotting paper and so on, recurring costs are limited to the expense for batteries and no bio-waste is generated. The device only requires annual maintenance.
In addition to haemoglobin, ToucHb also measures oxygen saturation, temperature and pulse rate. The cost of a test would be about Rs 10 or one-fifth the cost of conventional tests!
SaveMom: IoT-based maternal healthcare solution monitors pregnancies remotely
 |
|
Senthil Murugesan |
 |
When Senthil Murugesan, co-founder of JioVio Healthcare, visited his sister while she was pregnant in 2016, she was living on the outskirts of Madurai. She was often anxious about her pregnancy and would have to travel all the way to a city hospital for check-ups. Murugesan decided to visit her gynaecologist and ask about the vital parameters to be tracked for a pregnant woman.
He bought blood pressure and blood glucose measuring devices and replaced their display screens with a blue chip that would SMS his sister’s readings to the doctor, who would then evaluate them and message her back. The doctor would remind her to take the prescribed medicines and supplements and have a good diet. After his sister’s positive experience, it struck Murugesan that he could help many more women who had little or no access to healthcare facilities.
Globally, hundreds of thousands of women die preventable deaths every year due to pregnancy-related complications. In India, because many health departments are short-staffed, rural women are nearly three times more likely to die from complications during pregnancy or childbirth than those in urban areas. Many of these women are still wary of the modern healthcare system and cannot afford frequent visits to far-off hospitals.
While a mother’s death is a tragedy in itself, it has even worse cascading effects — her child is 15 times more likely to die before the age of two, and her other children may also die prematurely.
Murugesan set himself up to solve this problem. He developed SaveMom, an IoT-based maternal healthcare solution. SaveMom monitors a mother’s health using smart wearables that collect various physiological signals (blood pressure, heart rate, temperature, respiratory rate, ECG, oxygen saturation and glucose) continuously. These signals are processed with advanced techniques and a risk assessment is done continuously to ensure that she is healthy. The vitals are uploaded in the cloud for doctors to view remotely.
Caregivers and doctors are alerted if any mother’s risk assessment is negative, so that preventive measures may be taken at the right time.
The innovation consists of Allowear, a unique jewelry-inspired wearable device with six months of battery life. It tracks sleeping and steps taken, and provides reminders for medicines. It was specially designed to discourage men in the pregnant woman’s household from using it — which commonly happens with wearables in rural homes.
The second component is Allotricoder, an integrated non-invasive device that captures six vitals — blood pressure, heart rate, temperature, respiratory rate, ECG, oxygen saturation and glucose — digitally and sends the information to an AI engine for analysis.
The third component is AlloBMI, a simple weighing scale integrated with the application to monitor the steady rise in weight during pregnancy. This was especially necessary for rural areas where women astonishingly lost weight during the course of pregnancy, leading to unnecessary complications.
SaveMom has successfully addressed data manipulation malpractices of healthcare workers by ensuring that vital information can only be collected in the homes of the pregnant women after synchronizing the wearable devices to a mobile application. This ensures that the health worker visits a home every two weeks. The collected vital information can be sent to the doctor in real time for feedback.
JioVio has collaborated with local government agencies and NGOs for providing 1,000 days of care to mother and child for Rs 1,000 that covers 15 ante-natal check-ups for the mother and post-natal care for the baby. The solution has been deployed in over 100 villages in the southern states and benefited thousands of pregnant women by conducting tens of thousands of ante-natal check-ups.
There has been positive impact on the health of babies as well. For example, most babies born in the tribal region of Wayanad were underweight, so JioVio developed an innovative method to deliver nutrition to the rural mother using a drinking water source.
anuPath: Handy diagnostic tool to track diabetes and related problems
 |
| Vinay Kumar |
 |
Vinay Kumar, co-founder of PathShodh Healthcare, lived in a remote village in western UP where the health facilities are not up to the mark even today. At the age of 14, he was diagnosed with a chronic condition called juvenile diabetes — a sad turning point for both him and his family.
He had to take daily insulin injections to manage his illness. There was no doctor or testing facility in his village and no one in his family had even heard about juvenile diabetes until that point!
Kumar’s childhood experiences taught him the importance of science and motivated him to pursue research in public health and chronic disease diagnostics.
His mission eventually led him to set up PathShodh Healthcare. The company was incubated at the Centre for Nano Science and Engineering (CeNSE) at the prestigious Indian Institute of Science in Bengaluru.
Kumar and his colleagues developed anuPath, a point-of-care biosensing device that can measure multiple parameters related to diabetes, chronic kidney disease, anaemia, malnutrition and protein deficiencies. What’s more, it does not need special storage conditions and is ultra low-cost — 80 percent cheaper than conventional testing methods!
Globally, 425 million people suffer from diabetes and 1.6 million deaths are attributed directly to the chronic disease each year. It causes serious health issues, including blindness, foot amputations, heart attacks, chronic anaemia and kidney failure. anuPath is a pioneer, bringing the power of the hbA1C test in monitoring diabetes to the point of care.
Axiostat: Advanced wound dressing that stops heavy bleeding in two minutes
 |
|
Leo Mavely |
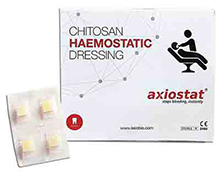 |
Around 40 percent of road accident deaths result from bleeding and there are 150,000 road accident deaths annually in India.
About 10 years ago in Delhi, Leo Mavely was a volunteer for efforts to help road accident victims reach hospitals in time. One day, he witnessed an accident in which a bus hit a bike, leaving the rider bleeding profusely.
Luckily, Mavely managed to take the victim to hospital in time and he survived. However, after watching the victim bleed profusely on the way, Mavely recognized the need for something revolutionary that could stop high-pressure bleeding and would save lives and, in the process, advance healthcare in India.
He did some research, but couldn’t find a single product in India that would stop such bleeding instantly. First responders only used gauze with high pressure, which is not enough for severe bleeding.
Mavely decided to explore biomaterials for a possible solution to prevent blood loss through open wounds during the golden hour: the one-hour period after an accident when a victim’s chances of survival are believed to be the highest.
In 2008, Mavely launched his company, AxioBiosolutions, to address this gap. He developed Axiostat, an advanced wound dressing that stops traumatic external bleeding. It utilizes the unique biomaterial, Chitosan, in a novel sponge form. It is India’s first developed, patented and commercialized emergency haemostatic dressing. It works on a unique charge-based mechanism of mucoadhesion which forms a mechanical barrier on the bleeding site.
The dressing is gamma sterilized, painless, and even works on patients on blood thinners. The versatile dressing can be cut, folded and stuffed into deep wounds — and it has no side effects. A key feature is the speed with which it stops bleeding — while standard gauze takes over 13 minutes, Axiostat takes just over two minutes to completely staunch bleeding!
With a presence in over 40 countries, AxioBiosolutions has today become a global name that uses innovative medical technology to create breakthrough products and save people’s lives.
Axio has a research collaboration partnership with Harvard Medical School to bring the latest scientific and technological innovations into the surgical and advanced wound care market. Advanced science and technology working for the disadvantaged!
3nethra: Comprehensive, cheaper eye test that makes dilation redundant, saves time
 |
|
Shyam Vasudev |
 |
When Shyam Vasudev visited Aravind Eye Hospitals to meet its famous founder, Dr Govindappa Venkataswamy, popularly known as Dr V, he did not know that it would change his life.
During his visit, Vasudev found that most eyecare equipment was imported, not portable and required a lot of power and expertise. Tests would take up to three or four hours. He decided to do something that would enable the wonderful doctors at Aravind Eye Hospitals to deliver better eyecare to people in the remotest corners of the country.
Thus, 3nethra was born — an intelligent, portable, non-invasive and low-cost device. It is also non-mydriatic, meaning it does not require pupil dilation, thus avoiding loss of working hours that a daily-wage worker can ill afford. It helps in pre-screening of five major eye diseases — cataract, diabetic retina, glaucoma and cornea and refractive index with powerful inbuilt auto-detection software.
More specifically, 3nethra is a digital fundus camera, equipped with an efficient workflow to capture high-resolution images of the eye through a quick-focus mechanism that reduces the examination time. It costs one-sixth of the current cost of collective pre-screening devices and can be operated by minimally trained personnel. The solution has a value proposition for everyone in the entire eyecare value chain from the elderly and rural poor to doctors, hospitals and entrepreneurs and pharmaceutical companies.
They currently have more than 3,350 devices in place in 45-plus countries and have screened more than eight million people with 75 percent of them being in India. Initially, they had only one version of the device which was used for adults and children above 10 years of age. Now, they also have several models and are in a position to screen all pre-term babies.
Dozee: Turns an ordinary hospital bed into a step-down ICU in a matter of minutes
 |
 |
|
Mudit Dandwate |
Gaurav Parchani |
It is estimated that India has only 1.9 million hospital beds and 95,000 ICU beds, three times less than the requirement. Most of the beds are concentrated in the private sector with substantial variation in available resources across states. While this has always been a healthcare problem it became even more critical during the COVID-19 pandemic. In addition, ICU beds are neither accessible nor affordable for a vast majority of the population.
An alumnus of IIT Bombay, Mudit Dandwate was actively involved in designing race cars before inventing Dozee. In fact, Dozee monitors the micro vibrations in one’s body in much the same way as vibration sensors are used to check the health of cars. Dandwate was working in an automobile company in Germany, when he came up with this idea.
“I was away from home and my parents’ health was always at the back of my mind,” he recalls. On his 24th birthday, he decided to resign and come back to India. His concern for his parents led him to devise and manufacture a health monitor. He roped in Gaurav Parchani as co-founder and Pritish Gupta as chief operating officer.
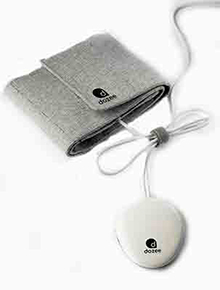 Dozee is a continuous, contact-free vitals monitor with remote monitoring capabilities and an alerts system that converts any bed into a step-down ICU in less than two minutes. Priced at less than Rs 9,000, it is about one-tenth the cost of conventional alternatives. Kept under the mattress, Dozee monitors patients’ heart rate, respiration rate, heart rate variability, oxygen saturation levels, blood pressure and activity levels through technology based on ballistocardiography. The device also lets clinicians set thresholds to trigger alerts for body vitals.
Dozee is a continuous, contact-free vitals monitor with remote monitoring capabilities and an alerts system that converts any bed into a step-down ICU in less than two minutes. Priced at less than Rs 9,000, it is about one-tenth the cost of conventional alternatives. Kept under the mattress, Dozee monitors patients’ heart rate, respiration rate, heart rate variability, oxygen saturation levels, blood pressure and activity levels through technology based on ballistocardiography. The device also lets clinicians set thresholds to trigger alerts for body vitals.
The device has medical-grade accuracy of 98.4 percent — as accurate as ECG, 2D Doppler Echo, RIP Bands. The data is uploaded to the cloud to afford remote access for clinicians. The data is further analyzed using advanced machine learning and artificial intelligence algorithms to profile the user. Setting up Dozee requires minimal technical expertise and it can be used in home settings. It can help reduce the workload of healthcare staff by almost 50 percent and provide proactive care.
In COVID times, thousands of beds were enabled with health monitoring, helping patients across seven states in India. Dozee is in use in 300 hospitals and 6,500 beds have been converted to step-down ICUs. Around 150,000 nursing hours have been saved by Dozee.
Dandwate set up an aspirational MillionICU initiative. It has received support from a large international public health organization to introduce continuous remote monitoring and AI-based early warning systems for 6,000 beds — beginning with 500 beds in Nepal, Bangladesh and Tanzania. Dozee is becoming an iconic global inclusive innovation.
PROPELLING INCLUSIVE INNOVATION
The power of inclusive innovation is infinite. My heart warms on seeing young, educated scientists, technologists and entrepreneurs commit themselves to this cause.
What do we now need to ensure that this movement gains momentum? Venture capitalists should not only look at three-fold money multiples but also three-fold life multiples. Can we prolong healthy life for millions of people? Can we give them a second chance to enjoy life to the fullest? Can we bring a smile to the faces of those in pain? All this is possible, if our head listens to our heart.
Second, there must be new financial instruments to support such inclusive innovations. The Anjani Mashelkar Foundation doesn’t just give awards but does everything possible to take innovations to the marketplace so that great ideas have an impact.
For example, when Tata Trusts were approached for support for the Sanket ECG device so that it could be perfected from a six-lead device to a 12-lead one, it took the trusts no time to write a `48 lakh cheque, and that too not as a loan but as a generous grant.
The Biotechnology Industry Research Assistance Council or BIRAC is doing a commendable job in incubating and supporting such inclusive innovations. Corporations now need to give a helping hand and take some risks by betting on the passion of these inclusive innovators, who want to do well by doing good.
What is required is compassionate capitalism, which can take different forms.
Corporations have so far done CSR 1.0, that is, doing well and doing good. In other words, become rich first and then support a societal cause.
But what we need now is CSR 2.0, which is doing well by doing good. In other words, doing good itself as a business — say, an extremely affordable high-quality vaccine.
I proposed this concept of CSR 2.0 in my K.R. Narayanan oration in 2019. But earlier, in 2000, I had co-authored a paper with C.K. Prahalad titled “Innovation’s Holy Grail: More from Less for More” for the Harvard Business Review, in which we set out a strategy for corporations to do well for themselves by becoming profitable while doing good for society.
We can also support inclusive innovation through the use of CSR funds in team India fashion. Dozee, the much needed step-up ICU, had a challenge in deployment even as people were dying in ambulances due to the huge shortage of ICU beds. Why? Public hospitals could not buy them due to lengthy tendering processes. Donations flowed in from around the world and that is how Dozee was installed across hospitals in India.
We need public-private partnerships in which funds come from CSR and the public sector helps with policies, infrastructure, regulations, and so on.
It is important for the government to support inclusive innovations through public policies. Tax exemptions, excise duty reductions, massive public procurement support for early-stage market seeding and market expansion are needed.
India created a world record by raising the share of LEDs in lighting from 0.2 percent to 88 percent in seven years through innovative demand aggregation and distribution/deployment. Can we not do this for diagnostics if CSR funds were pooled together, even regionally? Massive bulk purchases and deployment of such devices can be done on a huge scale across India. This could cause a paradigm shift.
India needs an inclusive innovation initiative. In this, scientists will have to be given special charters to work on cutting-edge science that leads to inclusion. They should be incentivized to create products with ‘affordable excellence’. Such an effort should be backed by systems and processes that will create acceptability and accessibility for the rural masses.
New matrices for judging individual as also institutional performance are needed for this purpose. The highest performance at the lowest price should be a goal that brings rewards. The ensuing competition will spark unconventional and bold thinking and will engender possible solutions for impossible-seeming problems.
Science and the excluded
 Anjani Mashelkar was a woman ahead of her time. More than seven decades ago, when it wasn’t easy to bring up a child singlehandedly, she was eking out an existence in Bombay, a big and unfamiliar big city to her.
Anjani Mashelkar was a woman ahead of her time. More than seven decades ago, when it wasn’t easy to bring up a child singlehandedly, she was eking out an existence in Bombay, a big and unfamiliar big city to her.
Poor, widowed and uneducated, she brought up her young son against many odds.
Raghunath Anant Mashelkar went on to have innumerable achievements in the world of science. And when he wanted to honour the courage with which his mother had groomed him, he set up the Anjani Mashelkar Foundation in her name after her passing.
The foundation’s focus is on institutionalizing and integrating science, technology and innovation to benefit people who live in poverty. Its mission is to promote inclusive growth through technology and science.
The Anjani Mashelkar Inclusive Innovation Award is a flagship programme of the foundation.
It recognizes and rewards game-changing inclusive innovations that are characterized by extreme affordability and high technology and can be scaled up sustainably with speed.
The award honours those who create not just ‘best’ practice, but ‘next’ practice. The foundation has recognized 13 innovations over the past 11 years.
The foundation helps awardees in their journey from ‘ideas to impact’. It supports them by making critical interventions in upgrading of technology, fundraising, opening doors for partnerships and scaling.
Dr Raghunath Anant Mashelkar is an influential thought leader who is globally recognized and honoured for his contributions to science and technology.
Comments
Currently there are no Comments. Be first to write a comment!



