
Smart urban PHCs: The Nagpur model
Umesh Anand, Nagpur
It is a morning like any other at the primary health centre at Futala. A large number of patients have turned up. They occupy steel chairs in the waiting area. A flat-screen TV on the wall keeps them entertained. Nurses in uniform are on duty. A peon, lean and distinctive in his crisp white topi, flits around on constant vigil. A laboratory attendant collects blood samples. Stocktaking is underway in the pharmacy. Machines that are part of a cold chain for vaccines are being checked out.
In her room, Dr Renuka Yawalkar, medical mask in place, comforts an elderly patient. Babybai Wasantrao Chalwankar is 70 and has been coming to Dr Yawalkar for four years. Her complaints are invariably minor ones — cough and cold, fever, headache, joint pains. Medicines help, but what really works is the companionable conversation with the doctor.
“She indulges me like a daughter would and puts up with my nonsense. She is always willing to listen,” says Babybai of Dr Yawalkar when we get talking later. “Sometimes I’m irritable and short-tempered, but she doesn’t mind.”
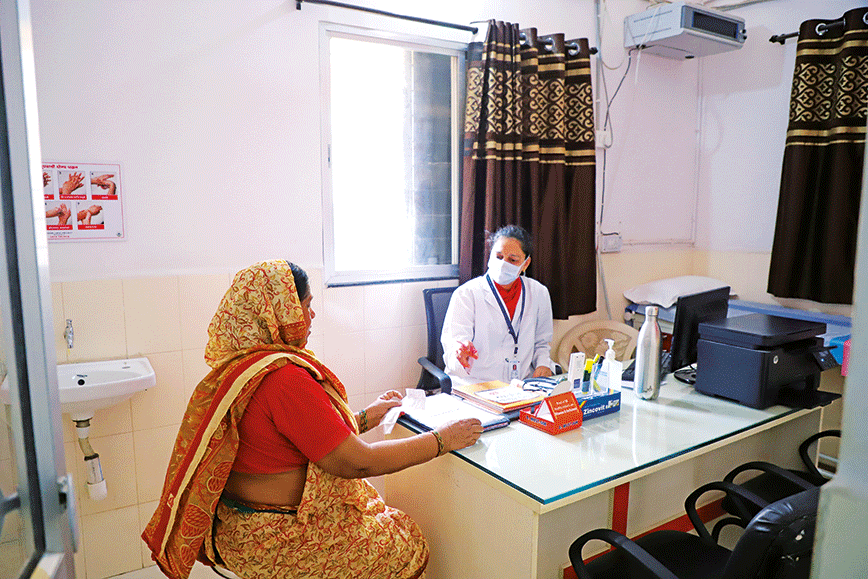 Dr Renuka Yawalkar comforts Babybai at the Futala primary healthcare centre | Photograph by Shrey gupta
Dr Renuka Yawalkar comforts Babybai at the Futala primary healthcare centre | Photograph by Shrey gupta
Futala is a slum in Nagpur. It is congested and squalid and notorious in the way slums tend to be. Babybai has lived here since the time there were a few houses and a pond and the area was nowhere close to being the urban sprawl that now exists. Her husband is a barber who works from the pavement. Her three sons have done better for themselves. Two are barbers like their father but they have got off the pavement and have a saloon each on rent. The third son is an attendant in a petrol station.
Hers is a family that has been moving up — not exactly middle class, but on its way there. The sons and their wives and children go to private clinics. Babybai and her husband prefer to come to this health centre run by the municipality. Being senior citizens, the couple isn’t charged for consultation or medicines. It is not as though those who have to pay are charged much. At just Rs 10 per visit, the health centre is as good as free for everyone.
The Futala facility is one of 26 urban Primary Health Centres (PHCs) that the Nagpur Municipal Corporation (NMC) has set out to revive with the support of the Tata Trusts. It is happening under the National Urban Health Mission (NUHM). In the past year, 17 PHCs have been upgraded in multiple ways. They have been repainted and given standard interiors. New furniture has been installed. The doctor’s room has been air-conditioned. With minimal changes in structure, the PHCs have undergone a transformation.
 The waiting area with patients and a peon on duty | Photograph by Shrey Gupta
The waiting area with patients and a peon on duty | Photograph by Shrey Gupta
Each PHC has been given computers and is networked. A patient’s record — symptoms, doctor’s advice, medicines prescribed and test results — are digitally stored. Some laboratory tests are done at the health centre itself. For the tests it can’t handle, samples are collected and sent to a central laboratory, which provides the results online.
A patient’s records are readily available on the doctor’s computer and are referred to on each visit. Once the 26 PHCs are all upgraded, information will be shared across them. A patient will then be able to consult a doctor in a PHC in any part of Nagpur. Ultimately, it is hoped these records will also be accessible in government hospitals, which would be particularly useful during emergencies or when providing specialised treatment.
Information technology has speeded up change. The use of computers was at first resisted, but is now welcomed because it really does make work easier. Doctors and the other staff who use computers tend to feel more accomplished in a contemporary way. Dr Sarita Kamdar, the municipality’s health officer in charge of the PHCs, has begun holding her weekly meeting with the doctors through video-conferencing. It is a big thing for her and everyone else at the PHCs.
With computers have come transparency and better processes. A patient registers at the reception where a photograph is taken on a webcam and a slip is issued. There is a sense of formality. A system is in place. In the past, PHC staff would be lackadaisical, but now they have an incentive to shape up and keep pace with a new sense of purpose.
 Child health and nutrition are tackled | Photograph by Shrey Gupta
Child health and nutrition are tackled | Photograph by Shrey Gupta
Cleanliness and upkeep have made a huge difference to the ambience of the PHCs. The Tata Trusts sought professional advice on interiors and layout to provide a uniform facelift so that all the PHCs look alike. Earlier, they were dank and lacking in hygiene. Hooligans would rule over many of them, including the now shining one at Futala, and misuse the premises.
Brightening up the PHCs and improving their infrastructure has had some immediate and significant benefits. For instance, the doctors feel motivated to spend more time on the job seeing patients. Earlier they would spend literally just as much time as needed to mark their presence. But now, with air- conditioning and a friendly environment, they arrive at 8 am and stay until 4 pm. It is a sea change from what used to happen.
Improvements have also resulted in greater expectations by patients. In a short while they have gotten used to higher standards. There is a demand for services, which in turn compels doctors, nurses and others to keep their end up. The number of patients visiting the PHCs has risen sharply. Patients say the services and ambience are now on a par with private clinics and the charges are much less.
“I have been coming here for many years and have seen the changes that have taken place. My husband and I pay nothing because we are senior citizens,” says Babybai. “But others also hardly have to pay anything for such good services.”
Shankar Wankhede, 68, and Damlu Pehalwan, 67, are vocal admirers of the transformation at Futala and proudly say they collaborated to bring it about when Dr Yawalkar reached out to the community for support.
“Several nearby private clinics have had to close down after the improvements at this centre. Patients prefer to come here,” says Wankhede. "This lady doctor is so good and gives so much attention to patients that people in other localities have also started coming here to consult her. It is not just her, everyone working in this health centre treats patients like they are their own family.”
Wankhede remembers a time when the health centre was in a mess. “For many years, the local boys used to drink and hang out here. Fights would take place. Doctors would put in a token appearance and make excuses of having to attend meetings elsewhere,” he says.
 The cnetral laboratory where PHCs send samples for testing | Photograph by Shrey Gupta
The cnetral laboratory where PHCs send samples for testing | Photograph by Shrey Gupta
Different interventions have been done. Better medical practices were of course essential but by themselves these would not have been enough. It was equally important to create confidence in the minds of patients and change the public profile of a government facility. Innovations were called for.
Upgrading the infrastructure and improving interior design was one way of making the health centres inviting and more like private clinics. It led to an image change, which took the centres from being dismal and neglected to looking good.
A second and more interesting move was to reach out to the hospitality industry. The Tata Trusts roped in the Taj’s hotel management institute at Aurangabad to impart soft skills to doctors, nurses and attendants. They needed to learn to be welcoming and attentive in the style of hotel staff. If patients
could be treated like guests they would be more inclined to come to a government-run primary health centre. It was also motivational for long-ignored staff at the PHCs to go through such training. It took them beyond their humdrum lives and provided them the opportunity to define themselves differently as service providers.
 Dr Mrinal S. Dhurjad at the Somalwada PHC which is yet to be refurbished | Photograph by Shrey Gupta
Dr Mrinal S. Dhurjad at the Somalwada PHC which is yet to be refurbished | Photograph by Shrey Gupta
RAPIDLY GROWING CITY
Nagpur’s population is officially 2.5 million, which makes it a small city, but it is growing rapidly and it is estimated that it already has about 3.5 million people though that may not be the official number.
Most of the growth is happening in the unorganised sector with migrants living in slums. With the shift to the city, they have begun their journey into the middle class. They have rising incomes and aspirations. Meeting their health needs is a complex challenge. It involves figuring out what they suffer from and then providing facilities that are accessible, affordable and efficient. People pay big chunks of their earnings to go to private health facilities because the government’s health centres are not good enough.
 “Families end up spending up to 10 percent of their income on health,” says Ram Joshi, additional commissioner of the municipal corporation. “By improving the PHCs the idea is to provide reliable healthcare at an affordable cost.”
“Families end up spending up to 10 percent of their income on health,” says Ram Joshi, additional commissioner of the municipal corporation. “By improving the PHCs the idea is to provide reliable healthcare at an affordable cost.”
He points out that in addition to the PHCs, the corporation has three hospitals. There are also two medical colleges and a specialised cancer facility. A branch of the All India Institute of Medical Sciences (AIIMS) has also opened in Nagpur.
But the PHC is the first building block of a larger healthcare system. It has a vital role to play because it exists in the midst of the community and serves as both a sentinel and a service provider. If run efficiently, it reduces the number of patients going to hospitals with minor ailments. Hospitals can then concentrate on serious cases.
As urban populations rise, dependable primary-level care becomes more important. Lifestyle diseases like hypertension and diabetes have become widespread and affect people in slums and upscale areas of a city alike. The PHC is part of a systemic solution, which can pick up these trends and address them before they go out of hand.
People go to private clinics and hospitals because they can buy easy access and they think they are getting quality treatment. If a government facility like a PHC provides both, at a cheaper price, patients benefit of course but a larger and more stable system also falls into place.
For instance, Babybai in Futala knows for sure that she does not have diabetes or hypertension. She knows because she is regularly checked at the primary health centre. She can also tell you that her husband is a borderline diabetic and is hypertensive. She has never had malaria and he has had malaria. Their personal health records exist.
 PHCs have a patient feedback system | Photograph by Shrey Gupta
PHCs have a patient feedback system | Photograph by Shrey Gupta
A PHC picks up trends. It refers patients who need specialised treatment to hospitals. Embedded as it is within the community, a PHC will know if there is a sudden increase in the number of cases of cholera, dysentery, malaria or jaundice. It can alert the sanitation department. It tracks infant and maternal mortality, facilitates institutional births and flags cases of malnutrition. Typically it has 11 people in different roles. There is one doctor. In addition, Ashas, who are field health workers, go deep into the community. There are also ANMs or Auxilliary Nurse Midwives.
“My health centre serves about 44,000 people. Our outreach takes us to pregnant women, children and adolescents. We take the weight and height of children. ANMs and Ashas collect such information and put it in the computer here. Information regarding every patient is recorded. ANMs go regularly, according to a fixed timetable. I make visits for supervision,” says Dr Yawalkar.
“Births don’t happen here but we send mothers to hospitals and we monitor them before and after delivery. I visit homes when I go to our outreach stations. In all we have 22 stations in a month. We get a large amount of data on patients who are high-risk, hypertensive, diabetic, suffering from malnutrition. We also get patients with chronic diseases like tuberculosis and leprosy,” says Dr Yawalkar.
“At my centre most patients come with complaints of cold, cough, fever, hypertension and diabetes, diarrhoea and gastroenteritis. There are cases of infected wounds and STDs. We have TB patients whom we treat. But this centre is only for primary care. The man who came a little while ago couldn’t open his mouth. It could be cancer, but we can’t make the diagnosis. So I referred him to a hospital for an assessment and only after that can we tell the patient what the problem is,” explains Dr Yawalkar.
Doctors have a leadership role to play in making a primary health centre effective. They set the bar for others to aspire to. The three doctors at the Futala, Babulkheda and Somalwada PHCs are self-motivated women with good qualifications. They are in government service by choice.
Dr Yawalkar, 45, is a pediatrician by training who gave up private practice. She says: “I get professional satisfaction from working in the public healthcare system. This is where I want to be.”
 The spruced-up PHC in Babulkheda | Photograph by Shrey Gupta
The spruced-up PHC in Babulkheda | Photograph by Shrey Gupta
At Babulkheda, Dr Swati Gupta, 36, is a gynaecologist who applied for the job because she felt it would give her more time with her children. A gynaecologist is on call at all hours. The PHC job requires her to be there till 4 pm.
But in the year or so that she has been here what Dr Gupta perhaps values more is the exposure to a wide variety of cases and the acknowledgement she often gets in the street.
“I went to buy bananas from a local fruit-seller and he immediately recognised me as the doctor from the health centre. It feels good. It doesn’t happen in private practice,” says Dr Gupta.
The Babulkheda centre under Dr Gupta has done well. The number of patients visiting it has gone up from 50 to 60 a day to more than 100. In April 2018, the centre received 520 new patients. In March this year, the figure rose to 1,309.
At the Somalwada PHC, Dr Mrinal S. Dhurjad, 37, is waiting for the infrastructure improvements. This PHC is in the third phase of the upgrade and is an example of how bad the infrastructure at the PHCs used to be. It is cramped and dingy and in urgent need of a coat of paint. It is not computerised beyond registering a patient and providing a slip. Patients do come, around 600 a month, but the lack of facilities is telling.
Dr Dhurjad is a gynaecologist. She has been in government service for the past three years. She says: “Doctors should be dedicated to public health.” But another reason for her being here is also that she can manage home and her job better in this role. Her husband is an orthopaedic surgeon and runs a small hospital of his own. One of them needs to have time for the children. “It is the female who always compromises,” she says.
Such choices seem to work well for the PHCs. Qualified and public-spirited physicians opt to work in the public health system both because of personal reasons and the satisfaction they get from their roles. These doctors do much to energise the PHCs. It’s a win-win situation.
“The main challenge is motivation of the staff,” says Dr Kamdar. “In government service they don’t want to give much time.” Earlier, PHC doctors had only loose contracts under the NUHM. The doctors chosen now are more committed. They get a salary of Rs 45,000 and a better working environment.

Dr Kamdar has been in charge of the PHCs since February. But she has been a government doctor for the past 22 years. She is cheerful and brims with the joy of work. At the three centres we visit, she has an easy camaraderie with the doctors. She also believes in the larger significance of the well-functioning PHCs.
“Primary health centres are the most important thing in delivering healthcare to people at the grassroots,” she says. “They are people-friendly and everything is under one roof. We are reaching out to the masses instead of waiting for them to come to us.”
“Lifestyle diseases cut across all strata of society. The primary health centre helps us know what is happening and deal with it at an early stage,” she says.“Patients with diabetes and hypertension can be tracked.”
Dr Kamdar stresses that “many, many good things have come from the association with the Tata Trusts”. Earlier there were 50 dispensaries in Nagpur. They were nowhere on the scale of the current PHCs. Dispensaries did not have ANMs and Ashas. There was no registration for immunisation and ante-natal care.
There is scope, she says, to bring in NGOs to educate communities on diet and exercise. There is also the need to train PHC doctors to deal with metabolic disorders. It is important that they know their boundaries — when to prescribe medication and when to refer cases to specialty institutions.
 The Tata Trusts team in Nagpur is geared for action and an incessant search for solutions at the local level | Photograph by Shrey Gupta
The Tata Trusts team in Nagpur is geared for action and an incessant search for solutions at the local level | Photograph by Shrey Gupta
TATA TRUSTS' ROLE
“We are champions of public health in primary care,” says H.S.D. Srinivas, who heads health initiatives at the Tata Trusts. “If we can meet the 60 percent requirement that is there on the ground then we don’t need to clog big hospitals. By detecting and managing chronic diseases within the community we delay the progression of these diseases.”
The request to look at Nagpur came from Maharashtra Chief Minister Devendra Fadnavis’ office. But other reasons for choosing Nagpur were a somewhat proactive local administration and the tag of a Smart City, under a national programme for upgrading urban infrastructure using technology.

“We wanted to visualise what could be the public health scenario in a smart city. Would it ease the delivery of care? We had done a lot in rural areas and it was time to look at the urban poor,” explains Srinivas.
As a result, Nagpur is the first city to upgrade its primary health centres under the guidelines of the NUHM. The Nagpur model that has emerged is one of a kind with the Tata Trusts working with the existing government system and its staff.
The trusts have brought in technology by way of an IT platform, better design and management practices, upgraded soft skills and made small investments in water coolers and air conditioners.
Ownership has remained with the municipal authorities and a governing council consisting of local administration officials and a representative of the trusts has overseen the project and collectively taken all decisions.
The process began in 2017 with the Tata Trusts doing a survey to have an assessment. It was found that the average footfall in the primary health centres was just eight to 20 patients a day although private practitioners nearby were doing well.
“A lot of chronic disease patients were flooding the two medical colleges in Nagpur and those who could afford it were going to private guys,” recalls Srinivas.
But the survey also revealed that if a doctor was present in a health centre people would be ready to go to it. The problem was that the doctors would turn up for just a couple of hours and lacked commitment.
“We thought a better ambience would make a difference. We took eight centres and created a prototype. The city administration was very supportive and pitched in with whatever funds they had for civil works and we added an airconditioner, a water-cooler and some signage,” says Srinivas.
In the past two years, capacity-building has been done in all 26 primary health centres. Technology and infrastructure improvements have taken place in 17. A better ambience has meant that doctors stay from 8 am to 4 pm as they should. Training by the Taj’s hotel management institute has made the staff of health centres friendlier. And as a result, the number of patients showing up for treatment has risen dramatically.
For a Smart City, the Tata Trusts felt there should be a seamless transfer of data and patient experience. Doctors and nurses had to adapt to technology in addition to their clinical responsibilities.
The linking of the laboratory at each centre with a central laboratory, where tests are done and the results sent back online, came from a system the Tata Trusts had created in Hyderabad. It has made a major difference. Patients no longer have to go to private laboratories for their tests and then come back with reports. It now all happens in a loop, which includes the doctor.
Strengthening a government system without taking it over requires trust and patience. Much of the credit for the success of what has been achieved in Nagpur should go to the Tata Trusts’ young team based in Nagpur.
Faceless and unassuming, this team, led by Amar Ramadas Nawakar, 36, has worked its way gently around innumerable problems from one day to the next. In an open-plan office in the building of the municipality, Nawakar shares a large table with Tikesh G. Bisen, Shruti Ande and Rejesh Bose K. It is a team geared for action and the incessant search for solutions at the local level. Any learning from the Nagpur model should include the need for such an efficient interface.
Comments
Currently there are no Comments. Be first to write a comment!



