
How a district hospital saved a baby weighing 650 gm
Civil Society News, Nalgonda (Telangana)
Mamatha arrived at the Nalgonda District Hospital atop the fuel tank of her uncle’s motorcycle. She weighed just 650 grammes. She had been wrapped in a small sheet of cellophane and put in some kind of a folder.
Her mother at that time was fighting for her own life after the premature delivery in the 28th week of her pregnancy. She had high blood pressure and was bleeding.
The doctors at the small private hospital where the delivery had taken place felt they could save the mother, but not the premature baby. In a district town like Nalgonda, a baby weighing just 650 grammes had virtually no chance of survival.
Nevertheless, the baby wasn’t dead either. So, her uncle took her from one hospital to the next, transporting her as best as he could — on the fuel tank of his motorcycle. He was turned away the first time by the Nalgonda District Hospital because rules at government hospitals say babies less than 1 kg, who are very premature, can’t be admitted. But when the uncle returned to the government facility and pleaded for a second time, having done the rounds of private hospitals, it was decided to take the baby in — if for no other reason than to give her a place to die.
That was on 30 December 2015. Six months later, Mamatha (very recently rechristened Rishita by her parents) is a healthy 2.3 kg. She is growing normally and her responses are just the way they should be.
In her dramatic survival is the script of the persistent efforts of the doctors and nurses of the Special Care Newborn Unit (SCNU) of the Nalgonda District Hospital as they went about saving the life of a baby who had been given up as dead even before she was born.
It was Mamatha’s destiny that she landed in the care of a medical team whose members shared a rare chemistry of purpose, professional values and great expertise. Her survival is proof of what government hospitals with public-spirited doctors can achieve. Very small babies like Mamatha have been saved, but only in tertiary hospitals. In a district hospital it is a rare feat.
Mamatha’s parents are poor and live with a larger family on just two acres of agricultural land. The mother’s name is also Mamatha, which is why the baby has now been renamed Rishita. The father is Shankar. They often work as farm labour. Mamatha and Shankar went to a small private hospital for the delivery because government services don’t reach people like them in distant parts of Nalgonda district. They spent Rs 60,000 on the delivery — money which had been saved and borrowed. By contrast, the excellent care mother and baby received for five months at the district hospital cost them nothing and saved the baby’s life in impossible circumstances.

State of the art facilities
Modern, efficient
The SCNU at the Nalgonda District Hospital is led by Dr Damera Yadaiah. At 52 he has spent almost 20 years in the government healthcare system and is as safe a pair of hands as you can get. A fit-looking man with a calm manner, Dr Yadaiah exudes experience and personal confidence. He is also passionate about serving ordinary folk who can’t pay fat bills in private hospitals.
Dr Yadaiah has put together a modern and efficient SCNU. He has been evangelical about benchmarking it with the best in the private sector. To him medicine is about serving society and it is this spirit that rubs off on his young team as well.
Though in a government hospital, Mamatha received the level of treatment she would have got at the best of private hospitals. For instance, as she arrived, she was given an injection of caffeine citrate to help her breathe. Mamatha was also administered what is called parental nutrition. This involves intravenously providing nutrients like glucose, lipids, dietary minerals and amino acids.
“Such care is expensive and usually given only in tertiary hospitals and corporate hospitals. But we gave the same care in our unit,” says Dr Yadaiah.
Mamatha was also put on CPAP, which stands for Continuous Positive Airways Pressure and helps the breathing of the baby. It is an alternative to a ventilator for which a tube has to be inserted. CPAP requires just two nasal prongs of half an inch.
“I didn’t think this baby would survive,” says Dr Yadaiah as we talk in his office over idlis and vadas. “So I kept CPAP for another baby. It costs Rs 7,000 to Rs 8,000 to administer and I didn’t want to waste resources. But the other baby succumbed and at the same time this baby was recovering, which came to me as a shock. It was purely a miracle.”
By the fourth day, these intensive measures had begun to yield results. When Dr Yadaiah went to see the baby she held his finger firmly, which made him intuitively feel that she was going to survive. It was now important to go all out to save her.
“In the first four days, I never had hope and felt they had unnecessarily admitted her. But then she held my finger, and with so much strength, that I was surprised. It was clear to me then that she would survive. I called my unit members and told them that we needed to support this baby in a big way. We have 20 babies and four nurses for each shift. So one nurse takes care of five babies. I told the nurses, do whatever you want, but one nurse will always be by this baby. This helped us in anticipating problems and responding immediately without any delay,” recalls Dr Yadaiah.
After 15 days, the doctors were really hopeful. But there were other complex challenges ahead. For instance, it was important to start feeding the baby from the mouth. Mother’s milk would have to be given, but pre-term babies can’t suckle. So milk was taken from the mother and put by tube directly into the baby’s stomach.
“We gave her mother’s milk, one millilitre every two hours. We gradually increased the amount of mother’s milk. After 40 days of feeding her through a tube, we started to feed her mother’s milk with a spoon and she also started accepting the spoon. The tube goes directly into the stomach but feeding from the mouth establishes gut flora and useful bacteria. From the spoon we graduated to a cup and finally after three months to breastfeeding.”
A serious difficulty the doctors faced was to get the family interested in Mamatha. She was a girl child and unwanted. A poor family didn’t want the burden of a sick girl child.
After her uncle had left her at the district hospital on the night she was born, the family came to see her only after 17 days. The mother didn’t return for a week after seeing her for the first time.
This presented a different kind of challenge for the doctors. A baby’s health is dependent on contact with the mother and the physical and emotional bonding between them. Also, since the mother was subconsciously rejecting the baby, she wasn’t lactating enough.
 Kangaroo mother care: babies born with low birth weight are held close by their mothers
Kangaroo mother care: babies born with low birth weight are held close by their mothers
Collecting mother’s milk
Mamatha’s nutrition had to come from mother’s milk. Faced with this situation, Dr Yadaiah began collecting milk from other mothers who were in the maternity ward of the hospital and producing surplus milk.
“I brainstormed with my team on what to do. If we gave powder milk there was the risk of losing the baby. As a solution we decided to opt for donor milk. But collecting it meant persuading other mothers. We go on rounds daily at 9 am in the maternity ward. I used to carry stainless steel boxes in my apron. I spoke to a few mothers who had given birth to babies very recently and told them that there was a baby who needed mother’s milk because her biological mother was failing to give milk. I requested them to give milk after their babies were done with breastfeeding each morning,” says Yadaiah.
It was the first time that Dr Yadaiah had done something like this. He used to take a nurse along who would help collect the milk. The milk would be put in containers with the donor’s name. Precautions were taken to check for hepatitis and HIV. But the mothers were kind and became involved in saving Mamatha, asking about her progress as the days went by.
Mother’s milk can last for six to seven hours without refrigeration. Dr Yadaiah has begun working on a plan for collecting what he calls “express mother’s milk” from branches of the Nalgonda District Hospital. The plan is to put the donor milk in containers and hand them over to bus drivers who will in turn hand them over to volunteers from the hospital.
Dr Yadaiah also had the tough task of convincing the mother that Mamatha would grow up normal and healthy. He showed her pictures of Babasaheb Ambedkar, Winston Churchill, Picasso and others and he explained that they were all born premature and underweight, but went on to be successful people. If Mamatha’s mother now holds her proudly it is because of all these efforts, which went much beyond medical interventions that are made in an ICU for pre-term babies.
Fixing the retina
The medical challenges in themselves were complex. Premature babies have to be screened for vision problems after 25 or 30 days. It is called retinopathy of prematurity or ROP, a disease in which abnormal blood vessels grow on the retina, causing it to detach and resulting in blindness.
Dr Yadaiah’s unit has an ophthalmologist who found a problem with Mamatha’s vision and there was a danger of her losing her eyesight if an intervention wasn’t done immediately. It was worrisome that Mamatha would live but be blind.
Dr Yadaiah consulted his friend, Dr Mereky Srinivas of Fernandez Hospital (See Civil Society Sept-Oct 2012) in Hyderabad who introduced him to Dr Subhadra Jallali of the L.V. Prasad Eye Institute. Dr Jallali drove down to Nalgonda with her laser equipment and an assistant. She spent five hours removing the abnormal blood vessels in Mamatha’s retina. Later, a second round of treatment was needed and for this Mamatha was taken to the L.V. Prasad Eye Institute in Hyderabad by car. Dr Jallali has said that Mamatha’s vision will be 80 per cent normal.
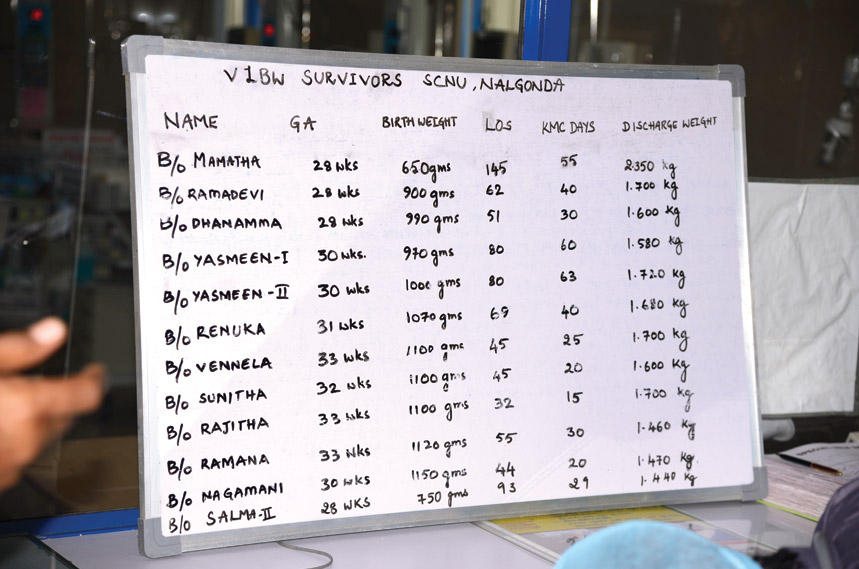 A list of premature babies who were saved
A list of premature babies who were saved
A baby’s development depends on connecting with the outside world. These connections happen while in the womb. But premature babies are born far too early to have this experience. For Mamatha a ‘sound spa’ was sourced from the US by one of the team members. It produces natural sounds like wind, rain, flowing water, thunder and so on. These sounds would be played for Mamatha and she began responding to them.
As Mamatha stabilised it was time to put her through kangaroo mother care. Mothers keep their babies on their chests like kangaroos do. It ensures the baby is warm and the constant physical contact promotes bonding and a feeling of security, which are essential to the baby’s growth. Initially, Mamatha received kangaroo mother care in the ICU itself. Later she and her mother were shifted to the kangaroo mother care ward where mothers and infants occupy two rows of beds.
A stonecutter’s son
Dr Yadaiah comes from a poor rural family in Nalgonda district. His father was a stonecutter. Dr Yadaiah and his siblings went to a village school some five kilometres from their home. They all went on to acquire higher education and have done well for themselves. Dr Yadaiah gained admission to the Gandhi Medical College in Hyderabad where he did his MBBS. He got a postgraduate degree in childcare from Nilofer Hospital.
He joined government service in 1998 and found himself posted in Nalgonda. In 2008 he suggested the setting up of a neonatal intensive care unit at the district hospital and with the help of his superiors got some funds from the district collector.
In 2010, when UNICEF began supporting hospitals to set up special units for saving newborns, Nalgonda already had one with 12 beds, the first in the country among government hospitals. UNICEF upgraded it to 20 beds in 2012 and provided better equipment. It is now funded under the National Rural Health Mission and has 14 nurses trained in tertiary care.
The Nalgonda District Hospital was also the first government hospital in the country to have retina screening for premature babies, kangaroo mother care and CPAP.
“Between 2008 and 2012 we discharged 3,000 plus babies. Post 2012 we have discharged 4,500 plus. So, overall the number of babies discharged goes up to 7,500 plus,” says Dr Yadaiah.
Initially, they would not take in babies weighing less than 2 kg. But they kept caring for smaller and smaller babies as the SCNU’s expertise grew. Finally there was Mamatha at just 650 grammes.
Nalgonda is a district known for poverty, water shortage and lack of infrastructure. Fluorosis is a serious problem in the district. In contrast, the SCNU that Dr Yadaiah and his team run is an island of excellence. The doctors and nurses are all products of government institutions and come from low-income families. Thanks to their efforts, Mamatha, the premature baby of very poor farm labourers, could get treatment and care that was state-of-the-art.
Comments
-

Neela D’Souza - Jan. 24, 2024, 6:26 p.m.
Inspiring and extraordinary . It should be widely read.



